Spider Veins Treatment Overview
What Are Spider Veins?
Spider veins, or telangiectasias, are small veins just beneath the skin’s surface formed by other damaged veins. They present most often on the legs or feet. Spider veins are typically red, purple, or blue, and form in clusters of thin lines that spread like webs or branches. A common underlying condition called chronic venous insufficiency is usually what causes spider veins.
What Causes Spider Veins?
Poor circulation is typically what causes the chronic venous insufficiency that leads to spider veins. Circulation issues originate in the deep veins that transport the majority of blood to the heart. These deeper veins are connected by perforating veins to the superficial, or saphenous, veins near the surface of your skin, which also transport a small amount of blood. One-way valves keep the blood flowing in the right direction, up and away from your feet. When these valves fail, blood heads back in the wrong direction, causing the superficial veins below the valve to swell. This additional pressure forces new spider veins to form.
Many factors contribute to valve dysfunction, which is why over 54% of women and 45% of men in America contend with spider veins or varicose veins, according to the Office of Women’s Health in America. Patient experience varies with spider veins, ranging from no discomfort to debilitating discomfort. Additional symptoms of spider veins include cramps, heaviness, restlessness, swelling, fatigue, and pain near the skin’s surface. Since venous insufficiency worsens with long periods of standing or sitting, most patients feel better when they change positions frequently and engage in consistent exercise.
Who Is at Risk for Spider Veins?
Like most health issues, spider veins become a greater risk as we age. Since hormone imbalances like high estrogen increase the risk, women are more susceptible to spider veins. However, incidence is high in both genders in adulthood. Additional risk factors include a family history of vein disease, history of blood clots, obesity, leg injury, birth control pills, pregnancy, hormone therapy, and jobs that require extensive sitting or standing. Of all the risk factors, a genetic predisposition or family history of chronic venous insufficiency is the most significant. If both of your parents had spider veins, your risk of developing them jumps to 90%.
What Causes Spider Veins?
Chronic venous insufficiency, or vascular disease, is the primary source of spider veins. The additional pressure it puts on your existing veins forces the formation of new, unhealthy spider veins. It’s similar to a pipe that leaks inside a wall, causing the liquid to disperse, staining the wall’s surface. These spider veins at the surface of your skin are the result of blood that was forced to spread out in a new direction.
What Are the Symptoms of Spider Veins?
Fortunately, the actual spider veins are often asymptomatic, primarily affecting our appearance. However, the venous insufficiency that causes them can produce many bothersome symptoms, like cramping, aching, burning, throbbing, heaviness, itching, swelling, or tingling in the legs. Patients with more severe cases of vascular disease might also experience changes in their skin and difficulty healing from ulcerations they develop.
How Do Doctors Treat Spider Veins?
If you aren’t in pain or experiencing notable symptoms, spider veins don’t necessarily require treatment. However, many patients still prefer to treat their spider veins for aesthetic purposes. In these cases, vein doctors offer simple solutions like sclerotherapy to eliminate the unwanted veins.
Which Vein Clinic Treatment Is Best for Spider Veins?
Before beginning spider vein treatment, seek a comprehensive vein evaluation from a board certified vein specialist. This is not only for your own safety, but also for treatment efficacy. If you simply treat the spider veins without determining whether you have venous insufficiency, your spider veins will likely return.
Sclerotherapy:
Physicians perform this simple procedure in-office. Sclerotherapy is remarkably safe and effective at removing spider veins. Doctors inject medicine into the veins individually, which irritates the vein’s walls, prompting them to close. Vascular disease makes unwanted veins appear, yet sclerotherapy makes them disappear.

Endоvеnоuѕ Lаѕеr Ablation:
Endovenous laser treatment offers a simpler and safer way to treat underlying venous insufficiency than vein surgery. Since it only requires local anesthesia, it’s performed in an outpatient setting and requires minimal downtime for recovery.
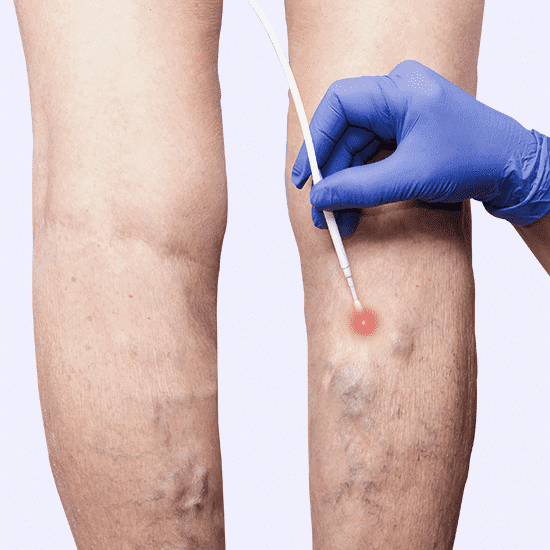
Radiofrequency Ablation:
The name of this procedure might sound ominous, but it’s actually a minimally invasive way to treat chronic venous insufficiency. Like laser ablation, endovenous radiofrequency ablation uses energy, in this case, thermal energy, to target the damaged veins directly. In comparison, radiofrequency ablation produces less bruising and discomfort than laser treatment.

Laser Therapy:
For those most concerned with the appearance of spider veins, skin laser therapy is a great solution. It’s most effective on the smaller veins, and works well in conjunction with, or as an alternative to sclerotherapy. Since it primarily targets the visibility of spider veins, it won’t improve symptoms of underlying venous insufficiency. Ask your vein doctor if it’s right for you, since some skin types don’t respond well to laser therapy.

Compression Stockings:
Also called support stockings, compression stockings are a simple home remedy for spider veins. The pressure they create helps pump blood up to the heart to prevent excess pooling in the veins. While they won’t eliminate the visibility of spider veins, they will help reduce the swelling and physical symptoms. Compression stockings are only safe and effective when fitted properly. See your vein doctor for a formal measurement and fitting before trying any type of support stockings.

Daily Exercise:
Like most health issues, daily exercise is one of the best defenses against spider veins. It not only prevents formation, it also helps alleviate symptoms by keeping your blood flowing smoothly in the right direction. When we’re active, the calf muscles help pump blood upward to the heart, enabling proper circulation. If you already have vascular disease, long periods of sitting or standing will only worsen your condition. Get plenty of exercise and elevate your legs above heart level while sleeping or sitting for prolonged periods to assist circulation.
